About Skin Problems
Skin problems are influenced by various factors, including sun exposure, genetics, hormonal fluctuations, medications, and underlying health conditions. Prolonged UV exposure can lead to premature aging, hyperpigmentation, and an increased risk of skin cancer, while genetics predispose individuals to conditions like eczema, psoriasis, and rosacea. Hormonal changes during puberty, pregnancy, or menopause often trigger acne, melasma, or oil imbalances. Certain medications, such as steroids and chemotherapy, can cause skin dryness, rashes, or pigmentation. Additionally, health issues like diabetes, thyroid disorders, and dermatological conditions disrupt skin health, leading to poor healing or inflammation. Exposure to heavy metals and environmental pollutants can worsen skin conditions, contributing to irritation and chronic damage. A proactive approach, including sun protection, balanced skincare, and professional consultation, is essential for managing and improving skin health.
Causes Skin Problems
Certain lifestyle factors can lead to the development of a skin disease. Underlying health conditions may affect your skin, too. Common causes of skin diseases include:
Bacteria trapped in your pores or hair follicles
Conditions that affect your thyroid, kidneys, or immune system
Contact with environmental triggers, such as allergens or another person’s skin
Genetics
Fungus or parasites living on your skin
Medications, such as the ones that treat inflammatory bowel disease (IBD)
Viruses
Diabetes
Sun
Bacteria trapped in your pores or hair follicles 🦠
When bacteria get trapped in your pores or hair follicles, it can lead to acne, pimples, or skin infections. These bacteria can cause inflammation and block the normal function of your skin, resulting in redness, swelling, and pus formation. Proper skincare and hygiene are essential to prevent bacterial build-up.
Conditions that affect your thyroid, kidneys, or immune system 🧠
Conditions such as hypothyroidism, kidney disease, or autoimmune disorders can significantly impact your skin's health. Dryness, rashes, and discoloration may occur due to hormonal imbalances or immune dysfunction. It’s crucial to manage the underlying condition to improve skin health.
Contact with environmental triggers, such as allergens or another person’s skin 🌿
Environmental triggers like pollen, dust, or contact with someone else’s skin can cause allergic reactions or irritation. This can lead to rashes, eczema, or hives. Avoiding triggers and using hypoallergenic products can help alleviate these skin issues.
Genetics 🧬
Genetics play a significant role in determining your skin type and susceptibility to certain skin conditions, like acne, eczema, or psoriasis. If your family has a history of skin issues, you may be more prone to developing them as well.
Fungus or parasites living on your skin 🍄
Fungal infections, such as ringworm or athlete’s foot, and parasites like scabies can affect your skin. These conditions may cause itching, redness, and rashes. Treatment typically involves antifungal or antiparasitic medications.
Medications, such as the ones that treat inflammatory bowel disease (IBD) 💊
Some medications, including those used to treat inflammatory bowel disease (IBD), can cause side effects like skin rashes, irritation, or increased sensitivity to the sun. Always discuss potential skin side effects with your healthcare provider.
Viruses 🦠
Viral infections, like herpes, chickenpox, or shingles, can cause various skin symptoms such as blisters, sores, and rashes. These conditions often require antiviral medications to manage symptoms and reduce outbreaks.
Diabetes 🍭
Diabetes can lead to poor circulation, dry skin, and an increased risk of infections. High blood sugar levels may affect your skin’s ability to heal and fight off infections, resulting in more frequent skin issues.
Sun 🌞
Excessive sun exposure can lead to sunburns, premature aging, and even increase the risk of skin cancer. It’s essential to protect your skin with sunscreen, wear protective clothing, and avoid long periods in direct sunlight to prevent skin damage.
- Bacteria trapped in your pores or hair follicles.
- Conditions that affect your thyroid, kidneys or immune system.
- Contact with environmental triggers, such as allergens or another person’s skin.
- Genetics
- Fungus or parasites living on your skin
- Medications, such as the ones that treat inflammatory bowel disease (IBD).
- Viruses.
- Diabetes.
- Sun.
Symptoms of Skin Problems
Skin disease symptoms vary significantly, depending on what condition you have. Skin changes are not always due to skin diseases. For example, you may get a blister from wearing ill-fitting shoes. However, when skin changes show up with no known cause, they may be linked to an underlying condition.
Generally, skin diseases may cause:
Discolored skin patches (abnormal pigmentation)
Dry skin
Open sores, lesions, or ulcers
Peeling skin
Rashes, possibly with itchiness or pain
Red, white, or pus-filled bumps
Scaly or rough skin
Raised bumps that are red or white
Fleshy bumps, warts, or other skin growths
Changes in mole color or size
A loss of skin pigment
Excessive flushing
Discolored skin patches (abnormal pigmentation) 🎨
These are areas of the skin that appear darker or lighter than the surrounding skin, often due to conditions such as hyperpigmentation (dark spots) or hypopigmentation (lighter spots). Causes may include sun exposure, hormonal changes, or skin conditions like melasma or vitiligo.
Dry skin💧
Dry skin, also known as xerosis, occurs when the skin lacks moisture and becomes flaky, itchy, and sometimes cracked. It may result from environmental factors like cold weather, low humidity, excessive washing, or certain skin conditions such as eczema.
Open sores, lesions, or ulcers 🩹
These are areas where the skin has been damaged or eroded, often accompanied by pain or fluid discharge. Causes can include infections, chronic conditions like diabetes, or trauma. Ulcers or lesions may also be a sign of more serious underlying issues like skin cancer or autoimmune diseases.
Peeling skin🧴
This occurs when the outer layer of the skin sheds in flakes or strips. It is common after sunburn, allergic reactions, or skin irritations, and can also be a symptom of conditions like psoriasis or eczema.
Rashes, possibly with itchiness or pain🌿
Rashes are inflamed or irritated areas of the skin that can range from mild redness to severe blistering. They may be itchy or painful and can result from various causes, such as allergies, infections, irritants, or chronic skin conditions like dermatitis.
Red, white, or pus-filled bumps 🔴
These bumps can be a sign of acne, folliculitis, or other skin infections. They occur when hair follicles become clogged or infected, leading to raised areas on the skin that may be painful or inflamed.
Scaly or rough skin 🏜️
Scaly skin is characterized by patches of skin that are dry, rough, and may flake off. This could be a result of conditions such as eczema, psoriasis, or fungal infections, where the skin cells multiply too quickly or fail to shed properly.
Raised bumps that are red or white ⚪
These can be symptoms of conditions like acne, hives, or folliculitis. The bumps may be inflamed or infected and could be accompanied by other signs like swelling or tenderness.
Fleshy bumps, warts, or other skin growths 🌱
These are often benign growths on the skin, such as warts (caused by viral infections), moles, or skin tags. While typically non-cancerous, any changes in size, color, or shape should be checked by a dermatologist to rule out more serious conditions.
Changes in mole color or size 🔍
Any changes in an existing mole’s color, size, or shape could be a sign of skin cancer, particularly melanoma. It is important to monitor moles for asymmetry, irregular borders, multiple colors, and growth over time.
A loss of skin pigment ☀️
This occurs when skin loses its natural color or pigmentation, leading to lighter spots, and can be a sign of conditions such as vitiligo, where melanocytes (pigment-producing cells) are destroyed.
Excessive flushing 😳
Flushing is characterized by sudden redness or warmth in the skin, typically on the face, due to increased blood flow. It can be triggered by emotional stress, temperature changes, spicy foods, alcohol, or conditions like rosacea.
Generally, skin diseases may cause:
Skin disease symptoms vary significantly, depending on what condition you have. Skin changes are not always due to skin diseases. For example, you may get a blister from wearing ill-fitting shoes. However, when skin changes show up with no known cause, they may be linked to an underlying condition.
- Discolored skin patches (abnormal pigmentation).
- Dry skin
- Open sores, lesions or ulcers.
- Peeling skin.
- Rashes, possibly with itchiness or pain.
- Red, white or pus-filled bumps.
- Scaly or rough skin.
- Raised bumps that are red or white.
- Fleshy bumps, warts, or other skin growths.
- Changes in mole color or size.
- A loss of skin pigment.
- Excessive flushing.

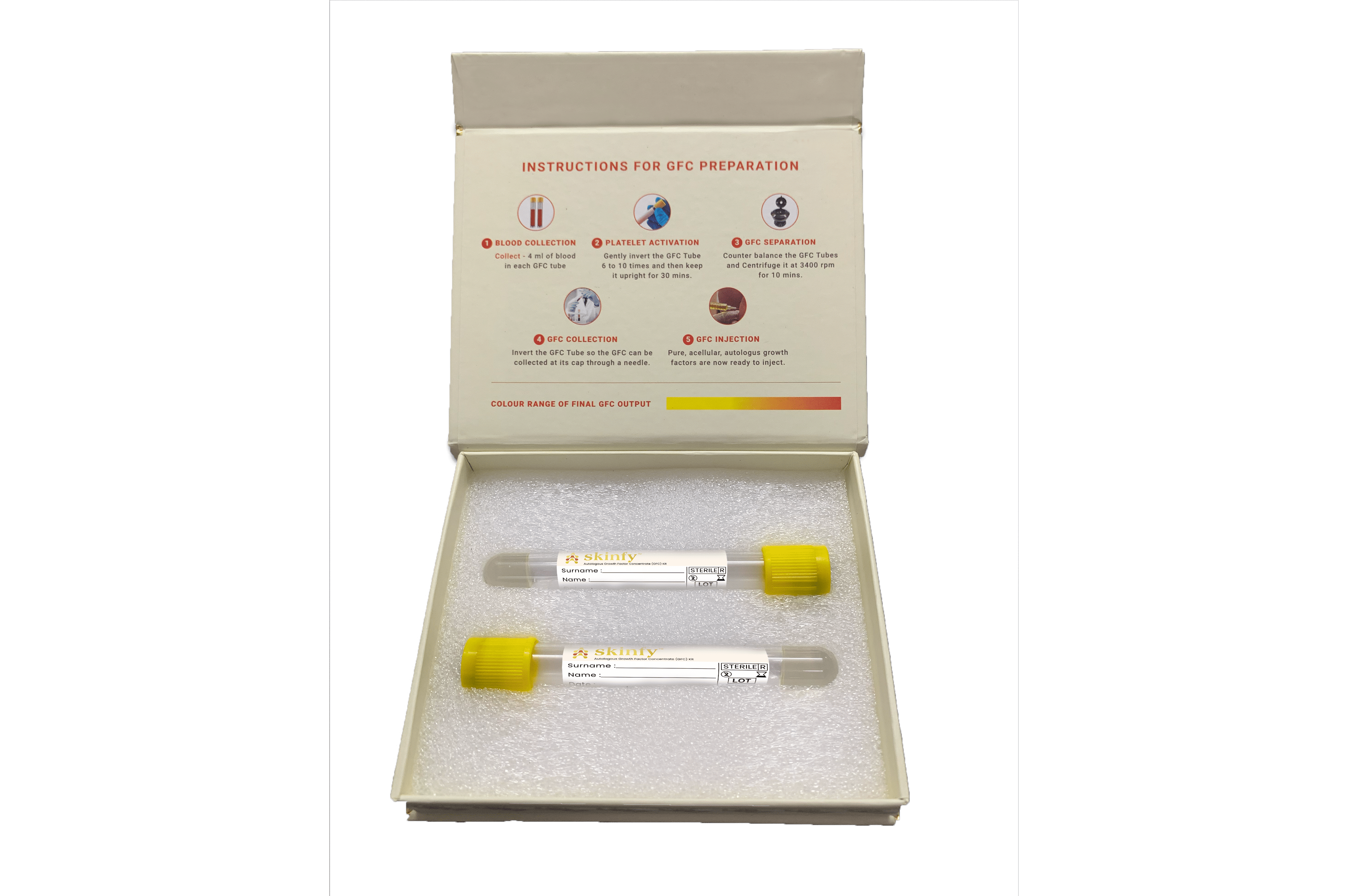
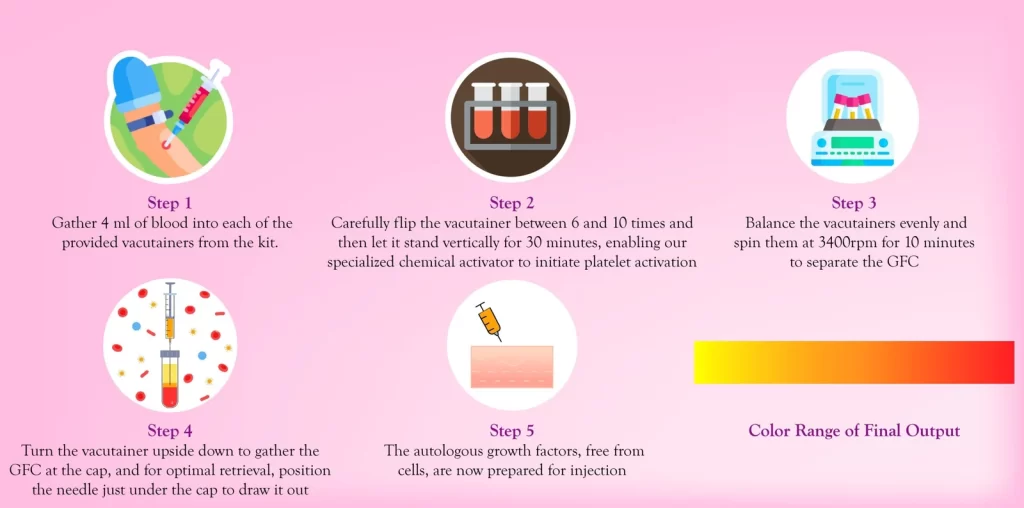
How to prepare GFC

Step 1 - Collection of Blood
Gather 4 ml of blood into each of the provided vacutainers from the kit.

Step 2 - Activation of Platelet & Release of GFs
Carefully flip the vacutainer between 6 and 10 times and then let it stand vertically for 30 minutes, enabling our specialized chemical activator to initiate platelet activation.
Step 3 - Separation of GFC
Balance the vacutainers evenly and spin them at 3400 rpm for 10 minutes to separate the GFC.

Step 4 - Collection of GFC
Turn the vacutainer upside down to gather the GFC at the cap, and for optimal retrieval, position the needle just under the cap to draw it out.

Step 5 - Application of GFC
The autologous growth factors, free from cells, are now prepared for injection.
Contact Us?
Address:
Kailash Tower, Vasai Link Road, Vasai Virar , Palghar, Maharashtra PIN 401209.
